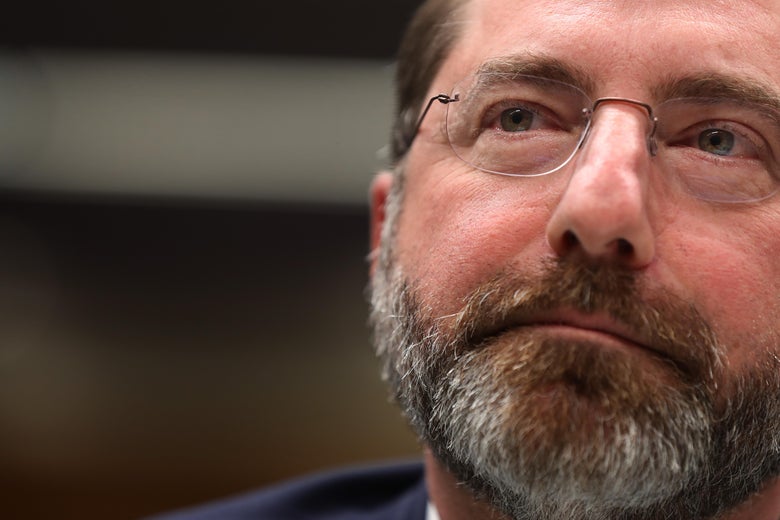
Health and Human Services Secretary Alex Azar testifies on Capitol Hill, Feb. 25.
Chip Somodevilla/Getty Images
In late February, as it became increasingly clear that the coronavirus was going to spread widely in the U.S., Health and Human Services Secretary Alex Azar told Congress, “we would want to ensure that we work to make [COVID-19 drugs] affordable, but we can’t control that price because we need the private sector to invest.”
We do need the private sector to invest. But the U.S. government is investing, too, and it deserves a say here, on behalf of taxpayers. Since the outbreak of SARS in 2002, the NIH has invested nearly $700 million in coronavirus research, and the first COVID-19 package passed by Congress included another $826 million for the development of coronavirus treatments, vaccines, and tests. All told, that means the U.S. will invest at least $1.5 billion in the development treatments and vaccines for coronaviruses. This research will then get handed off to private companies, which will finish development and patent their intellectual property—but we don’t know what they will spend. Without knowing that information, it’s impossible for the public to say what a fair price for them should be. A lot of evidence suggests that drug corporations could end up with a windfall, and that Americans may not see a fair return on our government’s investment in the form of fair prices. We probably won’t even know what the fair price is. We are hostages of our lack of information, and that makes our government a bad investor.
Transferring research to private corporations shouldn’t essentially be an open-ended blank check. The public should see some reward for their investment. We need an in-depth study of the costs of innovation to maximize the benefits and minimize the costs of our current drug discovery system. That could go a long way toward bringing down drug prices and increasing access for Americans—in the pandemic and beyond.
Public funding plays a huge role in drug discovery. One study found that every single drug of the 210 approved by the FDA from 2010 to 2016 started or benefited from research funded by the National Institutes of Health. The NIH invests about $41.7 billion annually in medical research, which is largely given in grants to more than 2,500 universities, medical schools and publicly funded research institutes.
Many people think that publicly funded research is responsible for the basic research, things like identifying the diseases pathways, and finding promises points of intervention, and the private market then does everything else, including the research needed to discover the drugs. But publicly funded research plays a big role in actual drug discovery. One study found a significant number of drugs discovered and patented through public funding, including 36 drugs to treat infectious disease. These also include those drugs that became many well-known and top-selling drugs like Allegra, Cialis, Humira, Botox, Lyrica, Enbrel, and Pepcid Complete. An estimated one-third of the NIH’s annual funding given to universities goes to clinical trials.
But we don’t know how much money private corporations need to invest to finish development to the point that a drug is available to patients. One study using industry self-reported data estimated these private costs at $2.8 billion, including failures. The most recent study estimated these costs at $985 million, and other studies have estimated as low as $314 million.
An understanding of how great of a role the public plays in drug development can also help us demand better deals when passing the torch from the public to the private. There are many examples of companies being accused of anticompetitive practices with drugs that were at least partially developed through public funding. Take Humira, whose method of treatment and formulation were at least partly discovered through public funding. The company behind it, AbbVie, built a wall of more than 100 patents to prevent competition on Humira until 2023. As a result, prices in the U.S. have been driven higher, while in other countries prices have come down significantly since 2018, when generics became available. The maker of Namenda, an Alzheimer’s drug, was successfully sued for product hopping by the state of New York. Restasis, a dry-eye drug, was the subject of a scheme to transfer patents to a Native American tribe to avoid a patent challenge by claiming sovereign immunity. In each of these instances, the U.S. public has been treated unfairly in purchasing drugs their taxpayer dollars helped fund the discovery of. It’s particularly galling because the profitability of large drug corporations is already almost double that of other large corporations.
For COVID-19 drugs, it is especially important that Americans get a fair deal, but that might not happen even when we do know how much companies are spending. For example, the nonprofit consumer advocacy organization Public Citizen examined government funding for COVID-19 treatments and found one contract where the Biomedical Advanced Research and Development Authority announced it would partner with a private company and pay 80 percent of the R&D and manufacturing costs. This is a substantial public investment. However, industry lobbying successfully removed language from the first COVID package that would ensure fair pricing.
Fortunately, there are lawmakers working on this problem. For example, last July Sens. Chris Van Hollen, a Democrat from Maryland, and Rick Scott, a Republican from Florida, introduced the We PAID Act, which would require private corporations that purchase publicly funded technology through the Bayh-Dole Act to meet certain fair pricing requirements. It’s an interesting idea that could be helpful in dealing with high drug prices. It also may take some time to gain enough traction to move. Fortunately, the bill includes a study to determine reasonable drug prices that can be separated from the main bill and should be passed now. This study would look at what reasonable prices should be in the U.S. when balancing things like how the costs and risks are shared, and what the return on investment needs are for drug manufacturers. At the very least, we should use this type of study to look at how COVID-19 drugs are jointly developed and ultimately priced.
Right now, our lack of transparency probably means we will end up giving the drug industry whatever they want to get COVID-19 drugs as fast as possible. But we don’t need to stay in the dark. Information gathering should be a key part of how we learn from this pandemic to better prepare for the future. Hopefully, that means being armed with the information needed to be good investors with our public dollars.
Future Tense is a partnership of Slate, New America, and Arizona State University that examines emerging technologies, public policy, and society.
from Slate Magazine https://ift.tt/3dyrwiX
via IFTTT
沒有留言:
張貼留言